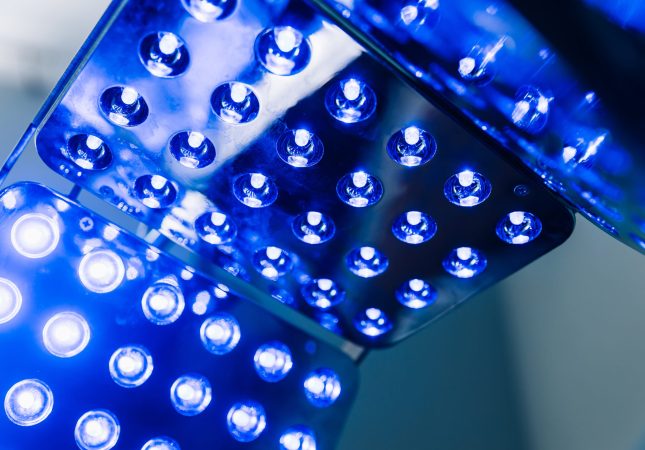
We’re still picking up the pieces after the COVID-19 pandemic. One of those lingering issues: aging UV-C devices.
The FDA gave a lot of leeway for UV-C disinfection in light of the situation, and many hospitals spent their COVID funding on purchasing them. But now, those devices are slowly breaking down due to lack of manufacturer support, and emerging FDA regulations further complicate the situation.
“I have been told by multiple hospitals that they are just ‘limping along’ with UV-C until the device dies,” says Peter Hoff, Nevoa VP of Sales.
We’re taking a closer look at the typical lifespan for UV-C devices and why so many hospitals are just getting by with dated disinfection technology.
Losing Manufacturer Support
UV-C vendors all claim different lifespans for their devices, some as low as two years and some reaching over ten. But as the device ages, the UV-C bulbs become less effective, with up to 20% reduction in output at the end of life stages.
The pandemic represents the first large-scale adoption of UV-C disinfection in hospitals, and now this early test case is experiencing the first large-scale need for maintenance.
As UV-C disinfection systems purchased with COVID dollars approach the end-of-life stage, many manufacturers no longer want to provide maintenance support.
They’re left only with the option to make do with dying UV-C devices or purchase a new system, without the injection of funding that came with COVID-19.
“Customers are feeling abandoned,” says Peter. “They’re stuck in a situation where they have an operational device today, but they won’t be able to make any major fixes. They’re just going to let it die.”
Does it make sense to replace UV-C disinfection?
It seems that most UV-C users will be left with one option: replacement.
During the pandemic, the FDA put UV-C approval on the sidelines in favor of getting more disinfection technology into hospitals. With the emergency precautions expiring, FDA authorization is required for UV-C disinfection systems to be marketed to hospitals.
Now that the FDA has stepped in to regulate UV-C disinfection devices, only two UV-C vendors have achieved authorization for only their latest devices. When it’s time to replace their dead UV-C device, hospitals will find that the system they’ve used for years no longer has approval for hospital use, sending them back to the drawing board.
As COVID-era UV-C devices start to run on fumes, hospitals are faced with a lot of questions about replacement. If hospitals opt to replace their UV-C devices, will this result in an unending cycle of device purchasing, degradation, and replacement? And without the pressure of the pandemic, now is the time to ask if UV-C is the best system for hospital disinfection, or if its shortcomings outweigh the benefits.
UV-C Disinfection Reduces the Lifespan of Other Medical Devices
Speaking of shortcomings, one of UV-C’s major downsides is that exposure to UV can accelerate degradation of other medical equipment and devices.
Plastics are especially susceptible to degradation due to UV-C exposure. As the lifespan of your UV-C device comes to an end, your other devices may not last as long as intended either, resulting in increased costs associated with frequent replacement.
UV-C vendors often recommend shorter cycles to prevent material degradation, but complete disinfection requires specific exposure times. UV-C disinfection may require up to 90 minutes to kill pathogens, depending upon distance from the surface and the intensity of the UV bulb.
Should hospitals choose between complete disinfection or the integrity of other medical equipment?
Replace UV-C with Stronger Disinfection Technology
If you’re faced with a UV-C device on its last legs, break out of the cycle and turn to disinfection without compromise.
Nimbus by Nevoa is an automated, whole-room disinfection system that makes rapid advanced disinfection possible, without the drawbacks of UV-C. Microburst, our EPA-registered HOCl fogging solution, is non-toxic, non-corrosive, and 80 times more powerful than bleach. Unlike UV-C, fogging reaches 100% of surfaces in the room to eliminate pathogens and reduce the risk of HAIs.
You also won’t be left behind by our customer support. Nevoa partners with your hospital to make sure your EVS and IP teams have everything they need to succeed. We offer a no-capital commitment option, and we retain the responsibility to repair, upgrade, and replace your fogging devices as needed.
Ready to stop “limping along” and step into the future of advanced disinfection? Reach out to Nevoa today to learn more.