Advanced disinfection solutions that use sophisticated technologies to eliminate viruses and bacteria have become critical in the healthcare setting.
While disinfection has always been a priority, the COVID-19 pandemic amplified the need to provide safe, sanitized treatment spaces for every patient. Today, those needs are even more apparent as everything from the rise of drug-resistant bacteria to prolonged hiring challenges have pressed healthcare providers to elevate their disinfection strategies.
In response, many healthcare facilities are turning to automated solutions to disinfect treatment spaces without inundating existing staff or compromising cleaning efficacy.
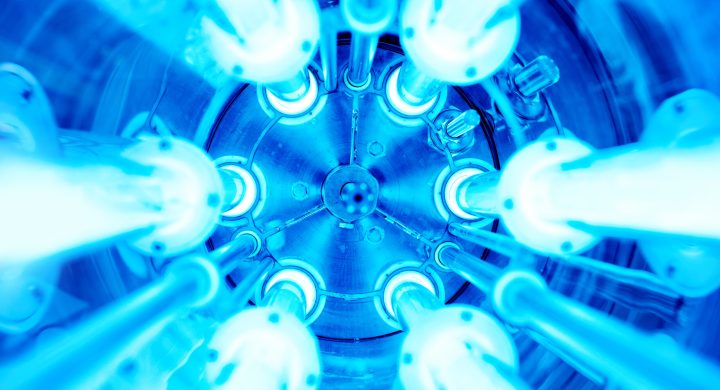
Often, this means adopting technologies that leverage UV to disinfect rooms. In theory, UV disinfection uses ultraviolet light, particularly its short-wavelength UVC range, to kill or inactivate microorganisms by disrupting their DNA, preventing them from reproducing and causing infections.
Many facilities choose UV disinfection due to a lack of knowledge about alternative solutions, some of which produce better results. Unfortunately, while UV may seem like the “easy” choice when it comes to advanced disinfection, this technology has surprising shortcomings that compromise its efficacy and diminish its impact.
Here are five shortcomings that hospital decision-makers need to know before integrating this expensive, well-known — but limited — technology into their treatment centers.
#1 UVC requires line of sight to be effective.
UVC’s effectiveness is contingent on proximity, making positioning (and repositioning) critical to its disinfection potential. Simply put, it can only kill what it shines on. Therefore, if the unit is placed on one side of an object, there’s a significant chance that the other side is “shadowed,” and won’t receive any UV light.
The absence of light exposure means the object or surface hasn’t been sanitized, making line of sight essential to its success. Not only will viable pathogens be left behind on untreated areas, these survivors can increase exponentially in a very short time.
To ensure maximum coverage and effectiveness, it’s imperative to reposition a UV unit several times to illuminate as many surfaces from varied angles as possible. This can be time consuming and cumbersome on hospital staff.
#2 UVC takes time to kill pathogens.
UVC disinfection takes time to work. While vendors quote different expected disinfection timeframes, healthcare providers leveraging the technology must account for several device repositionings, multiplying even the most ambitious manufacturer promises.
Think of UVC in terms of getting a tan in the sun. If you step outside for just five minutes, you won’t see much change in your skin. But if you lounge under the sun for an hour, you’ll probably get a tan, or even a sunburn. In the same way, using UVC for a quick five minutes won’t do much.
For instance, to effectively kill C. diff, UVC exposure might require up to 45 minutes in each room position due to the Inverse Square Law (detailed below), rapidly expanding the time needed to eliminate the most concerning viruses and bacteria.
#3 UVC effectiveness degrades quickly with distance.
Distance plays a critical role when it comes to the efficiency of UV disinfection. If a surface is two meters from the UV source, disinfecting it may take around 20 minutes. However, double that distance to four meters and you might be looking at a disinfection time of 40 minutes. Given the varying sizes of rooms, this can lead to much longer cycle times. When you factor in the need to reposition the UV unit multiple times, the entire disinfection process can take hours to complete.
This phenomenon can be better understood through the “Inverse Square Law,” a principle in physics that describes the relationship between the intensity of light and the distance from its source. Just like a sound wave is quieter when heard farther away from its source, UVC is less potent and impactful as it travels further from its source, limiting UVC’s reach in a healthcare setting.
To account for this shortcoming, some manufacturers are deploying expensive autonomous devices that automatically move around a predetermined space (similar to a self-propelled Roomba vacuum). While this theoretically automates the disinfection process, the incredibly high upfront costs, potential service demands, and limited proven efficacy make it a non-starter for healthcare providers already experiencing budget constraints and high demand for their treatment spaces.
#4 The EPA does not certify UVC
The EPA does not routinely assess the safety or effectiveness of UV light devices.
Thus the EPA cannot vouch for the effectiveness of these devices against pests, including viruses and bacteria. The effectiveness of UV light devices hinges on multiple variables, such as how long they’re used, their distance from the targeted surface, the UV wavelength, and the specific nature and strength of the pest being addressed.
That’s why the EPA warns users to “Be Careful With UV Lights or Ozone Generators” as “UV lights or ozone generators may be risky or ineffective.” Don’t be fooled by marketing that masquerades as certification, giving the impression that a UV product has been granted regulatory oversight when it has not.
#5 UVC causes material degradation.
Prolonged exposure to UV light can lead to the degradation of certain materials, including polymer surfaces, which are often found throughout treatment rooms in medical devices and equipment.
This deterioration can affect the structural integrity and appearance of these materials, leading to potential damages, fading, or even shortening their overall lifespan. It’s crucial to balance the benefits of UVC disinfection and its impact on the materials within its exposure range.
Hygienic Theater Won’t Improve Patient Outcomes
Advanced disinfection technologies, particularly UV-based solutions, have gained traction in healthcare settings due to their touted efficacy against viruses and bacteria. The urgency for stringent disinfection measures became even more pronounced during the COVID-19 pandemic, pushing healthcare providers to elevate their strategies and adopt automated solutions.
While UV disinfection, especially within the short-wavelength UVC range, has been a popular choice due to its ability to disrupt microbial DNA, it’s essential to recognize its limitations. From requiring a direct line of sight to be effective and extended time frames for disinfection to its diminished potency with distance, the potential for material degradation, and a lack of certification from agencies like the EPA, UV’s pitfalls are glaring.
While this hygienic theater might look and sound impressive, it won’t necessarily translate to tangible patient outcomes. Before adopting the latest, unproven UVC technology, let Nevoa revolutionize disinfection protocols in your healthcare facility.
Nevoa’s Nimbus offers whole-room fogging, and is distinguished as the sole hospital-grade system approved for fogging with EPA-registered hypochlorous acid (HOCl). This powerful solution provides unparalleled disinfection while allowing immediate room reentry and reducing manual labor outputs for nursing and EVS teams.
With no upfront capital required, Nevoa is ready to prove its efficacy in your environment. Request a demo and learn more about how you can try a proven advanced disinfection solution in your healthcare facility with minimal capital investment today.