Is your hospital prepared for this “urgent threat” that’s sweeping through U.S. healthcare facilities?
Candida auris is an emerging fungal HAI that is raising alarm bells due to its rapid spread and dangerously high mortality rate. But in spite of the headlines and concerns from healthcare professionals, many hospitals have been left without guidance to manage this threat.
Your hospital needs to know:
- What is C. auris?
- What to do in the event of a C. auris outbreak?
- What can you do to reduce the risk of a C. auris outbreak at your facility?
- How is C. auris spreading across the U.S.?
We’re here to help. Find out more about C. auris and how your hospital can proactively fight against this growing public health crisis.
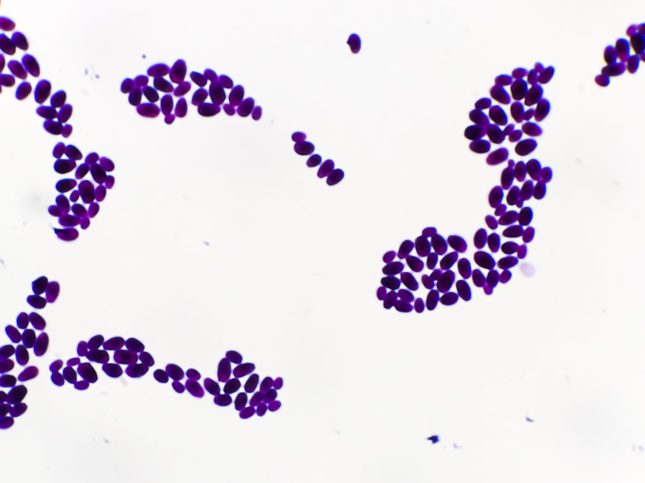
What is Candida Auris?
Candida auris, commonly known as C. auris, is a type of yeast that is making headlines as a deadly superbug. While first identified in the U.S. in 2016, the CDC believes that pandemic stress on the healthcare system allowed C. auris to spread rapidly as a healthcare-acquired infection.
C. auris spreads via person-to-person contact and through contact with contaminated surfaces, with the capability to live on surfaces and equipment for several weeks if not properly disinfected. And while it’s easy to spread, C. auris is extremely difficult to identify via laboratory testing, slowing response time for infection prevention teams.
Most concerning is the infection’s resistance to several antifungal treatments. With already limited treatment options, C. auris typically results in severe infections, weeks-long hospitalizations, and high mortality. Currently, the CDC estimates that 1 in 3 C. auris patients will die as a result of the infection.
How to Manage C. Auris Cases at Your Hospital
If C. auris is already a problem at your hospital, how can you minimize the spread? And how can you improve patient outcomes?
Here are a few ways that the CDC suggests to control the spread of C. auris once a case is identified:
- Isolate infected patients in single rooms with dedicated equipment and implement contact precautions
- Increase frequency of advanced cleanings in patient areas, especially in areas with reusable equipment (blood pressure cuffs, nursing carts, etc.)
- Enhance cleaning protocols with automated disinfection
- Use disinfectants that are known to eliminate C. difficile
- Re-emphasize hand hygiene protocols for faculty and staff
- Monitor other patients for signs of new C. auris cases
Preventing C. Auris Outbreaks
It’s not a question of if, but when a C. auris infection will occur at your hospital, but the best offense is a good defense. If your hospital has yet to report its first C. auris case, now is the time to get prepared.
It’s time to upgrade your cleaning and disinfection protocol to guarantee that every surface gets 100% disinfected during room turns. Unfortunately, manual cleaning leaves room for human error, like missed spots and recontamination. And there’s no room for error when it comes to this type of superbug.
“It’s really good at just being, generally speaking, in the environment,” says Melissa Nolan, University of South Carolina assistant professor of epidemiology and biostatistics.“So if you have it on a patient’s bed for example, on the railing, and you go to wipe everything down, if in whatever way maybe a couple of pathogens didn’t get cleared, then they’re becoming resistant. And so over time, they can kind of grow and populate in that hospital environment.”
Consider technology that automates your room disinfections, like Nimbus by Nevoa. Our whole-room disinfecting fogger removes the risk of human error and ensures that any C. auris spores are eliminated before they can populate your hospital.
The State of C. Auris in U.S. Hospitals
2025 has already been a year of increased C. auris cases. According to an April 2025 CDC report, C. auris has been reported in 17 U.S. states, including:
- Texas
- Michigan
- Ohio
- Virginia
- Arizona
- Colorado
- Delaware
- Illinois
- Indiana
- Iowa
- Louisiana
- Maryland
- Montana
- New Mexico
- Pennsylvania
- Utah
- Wisconsin
Even with this concerning increase in cases, more cases are likely going unreported. For many hospitals, the lack of solutions to manage and prevent C. auris response leads them to avoid testing altogether.
Nevoa’s own Peter Hoff, VP of Sales, spoke with infection preventionists at APIC 2025, and heard about their frustrations firsthand: “Some hospital infection preventionists shared that their facilities are not currently testing for C. auris, even though they strongly suspect its presence. They don’t want to sound the alarm until they’ve identified a viable mitigation strategy.”
The solution they’re seeking isn’t just a miracle antifungal treatment or a better disinfectant. Hospitals need guidance from partners they can trust and a plan of action to better control C. auris when it rears its ugly head.
Nevoa is here to be a partner and resource as your hospital navigates the spread of C. auris. Our rapid disinfection products have the power to eliminate C. auris from your equipment, surfaces, and even floors with just two minute contact time. Take the guesswork out of your infection prevention strategy, and put your trust in automated cleanings that leave no questions about complete disinfection, every time.
Reach out to us to learn more about proactive defense against C. auris.